Essentials steps of dental cleaning & therapy
Click on each step to learn more
1. Conscious oral evaluation
Perform an oral evaluation on the conscious patient before administering anesthesia. A visual assessment can suggest whether periodontal disease exists and its extent.
2. Anesthetized intraoral radiography
Radiograph the entire mouth of the anesthetized patient using intraoral film or intraoral digital radiographic systems.
3. Teeth scaling
Scale the teeth supra- and subgingivally using a hand scaler (supragingivally), curette (subgingivally), or an appropriately powered ultrasonic scaler followed by a curette inserted subgingivally to remove additional plaque and calculus (Figure 5). Do not use a rotary scaler, which excessively roughens the tooth enamel.39,40 Elimination of calculus is essential because it acts as a retention matrix for plaque and toxins harmful to the tooth’s support. Curettes are designed to assist in the removal of subgingival plaque and calculus for root planing and curettage (soft tissue removal in diseased periodontal pockets). Curettes have a smooth, rounded heel and toe opposite the cutting surface. The rounded back makes curettes less traumatic to soft tissues compared with sickle scalers.
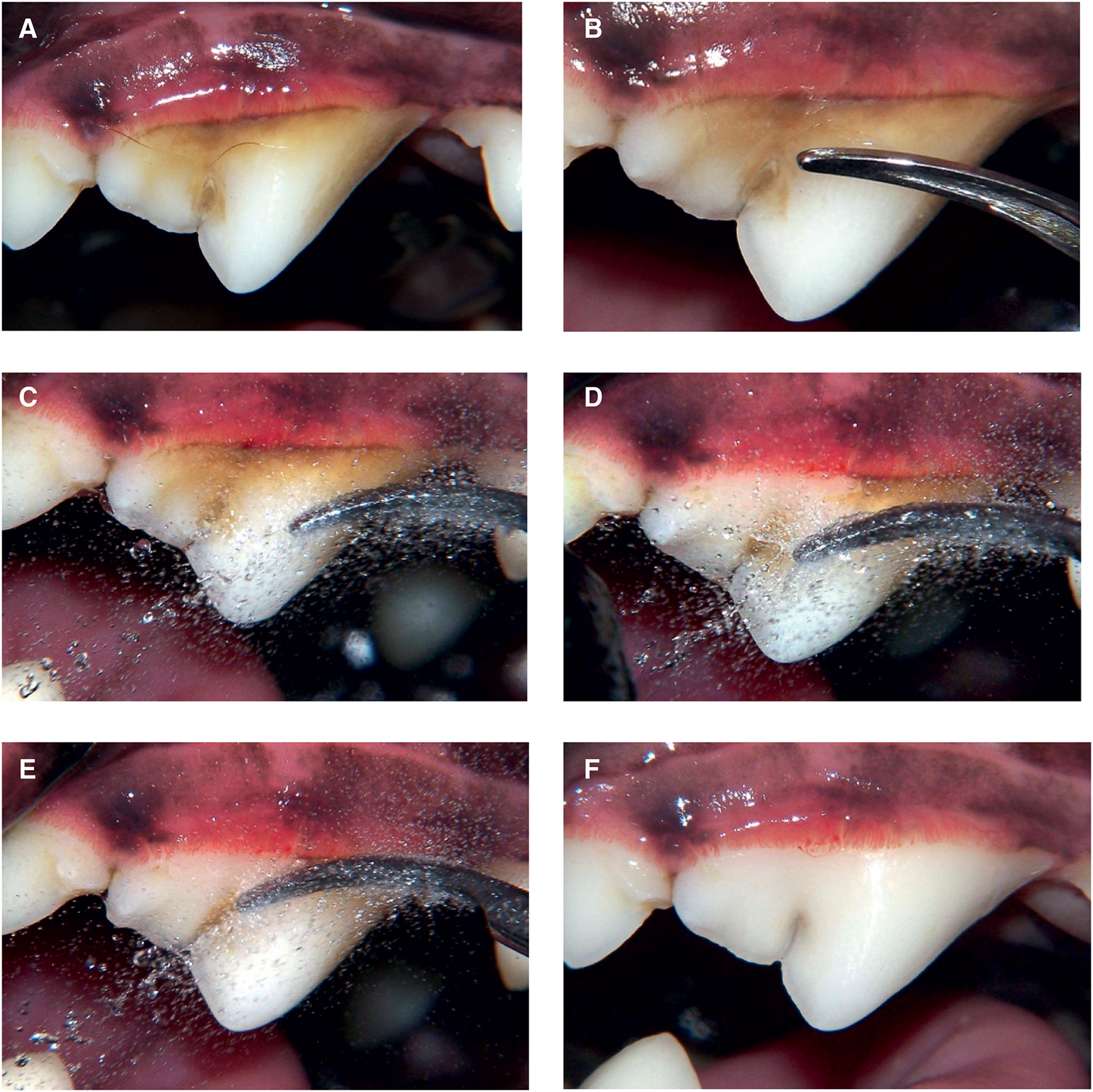
FIGURE 5 - Sequence for a dental cleaning using an ultrasonic scaler. Photo courtesy of Jan Bellows.
(A) Plaque- and calculus-laden right maxillary fourth premolar.
(B) Placement of the ultrasonic scaler tip against the crown before activation.
(C) Activation and tuning of the ultrasonic scaler to deliver a cooling and irrigation mist.
(D) Removal of plaque and calculus.
(E) Removal of plaque and calculus from the developmental groove.
(F) Cleaned tooth.
Do not use a rotary scaler, which excessively roughens the tooth enamel.39,40
Elimination of calculus is essential because it acts as a retention matrix for plaque and toxins harmful to the tooth’s support.
Curettes are designed to assist in the removal of subgingival plaque and calculus for root planing and curettage (soft tissue removal in diseased periodontal pockets). Curettes have a smooth, rounded heel and toe opposite the cutting surface. The rounded back makes curettes less traumatic to soft tissues compared with sickle scalers.
Every professional teeth cleaning should include hand scaling of the accessible root surfaces (Figures 6, 7). Aggressive curettage and scaling causing cementum removal is discouraged. Cementum covering the roots contains cell-activating proteins that encourage reattachment. Dentin does not contain these proteins. Subgingival ultrasonic treatment causes cavitation and disruption of the subgingival ecosystem and biofilm. The design and safety of thin, long, ultrasonic periodontal tips decrease the need to aggressively root-plane teeth affected by periodontal disease.

FIGURE 6 - Hand scaling of accessible root surfaces.
Photo courtesy of Jan Bellows.
(A) Orientation of the curette before placement in the periodontal pocket.
(B) Insertion of curette into the periodontal pocket.
(C) Removal of subgingival debris.
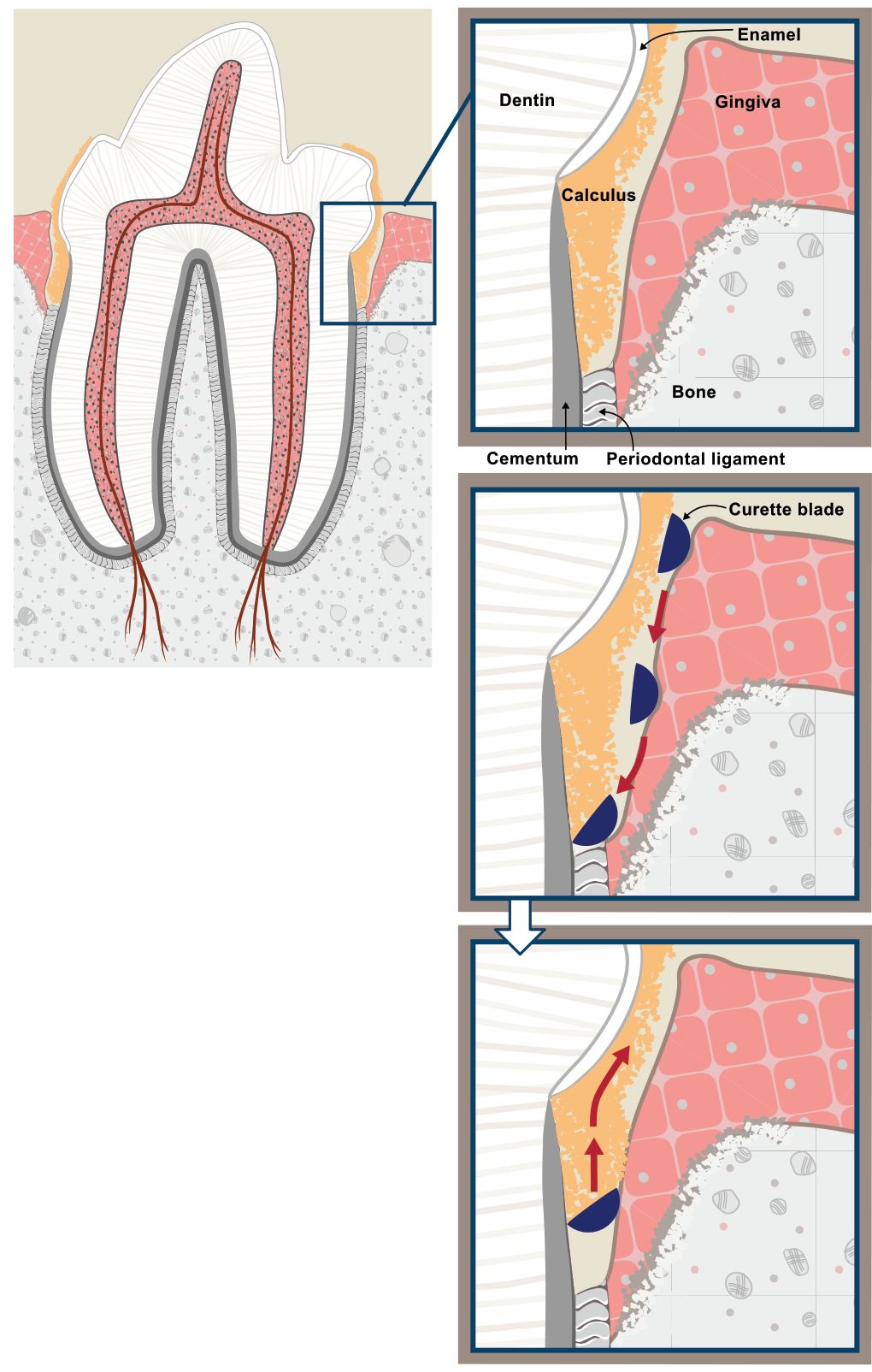
FIGURE 7: The subgingival curette blade is introduced atraumatically below the gumline with the face of the instrument nearly parallel to the root surface. At the bottom of the sulcus, the handle is adjusted, causing the down (cutting) edge of the instrument to contact the root surface. Plaque, calculus, and debris is removed on the upward pull stroke.
©2019 Veterinary Information Network (VIN), illustration by Tamara Rees.
4. Crown polishing
Crown polishing is recommended after cleaning and scaling, to assist in the reduction of microabrasions on the enamel. Polish the teeth using a low-speed hand piece prophy angle and polishing cup running at no more than 3000 rpm. Polish with prophy paste or fine-grit pumice because medium or course grit can contribute to enamel loss, microabrasions, and predisposition for plaque accumulation. The use of disposable prophy angles and individually packaged prophy paste is strongly recommended to avoid cross contamination.
5. Periodontal probing
Perform oral evaluation using a periodontal probe after dental scaling and full-mouth radiographs have been obtained. Each tooth should be probed in at least six places parallel to the roots. The probing depth should not be greater than 2–3 mm in a midsized dog and 1 mm in a midsized cat. Oral examination abnormal findings should be charted.41
6. Subgingival irrigation
Perform subgingival irrigation to remove debris and polishing paste and to inspect the crown and subgingival areas. Use the air or water syringe to inspect the visible subgingival areas for remaining calculus requiring removal (Figure 8).

FIGURE 8 Compressed air used to visualize the root surface and subgingival calculus. Photo courtesy of Jan Bellows.
7. Periodontal therapy or extractions
After sharing examination findings, a therapy plan, related fees, and informed consent with the pet owner, perform indicated periodontal therapy or extractions. Periodontal disease staging and appropriate treatment are as follows:
|
Stage 1 (PD1): Gingivitis Treatment: Dental scaling, polishing, irrigation, home dental care. |
|
Stage 2 (PD2): Early periodontal disease with <25% attachment loss Treatment: PD1 care plus locally applied antimicrobials and/or subgingival scaling if pocketing exists. |
|
Stage 3 (PD3): Established periodontal disease with 25–50% attachment loss Treatment: Periodontal therapy* including periodontal surgery will only be successful if the client is committed to consistently administering home dental care. Extraction indicated if client and patient will not commit to daily home oral hygiene. *Periodontal therapy: closed- or open-root planing ± locally applied antimicrobials or advanced periodontal treatment such as guided tissue regeneration. |
|
Stage 4 (PD4): Advanced periodontal disease with >50% attachment loss Treatment: Extraction or periodontal surgery including osseous resective or additive procedures followed by consistently performed home dental care; prognosis is considered guarded. |
Extraction site packing, which includes bone autografts, allografts,or synthetic products, may be appropriate in select extraction sites where the remaining supporting bone is at risk for fracture during the period of extraction site healing, for example, in a dog’s mandibular first molar or canine. These products are used to facilitate bone healing when concern over bone integrity or strength exists. The use of extraction site packing is contraindicated in the presence of osteomyelitis or infection.42–44
Periodontal surgery is performed to remove deep debris, eliminate pockets, and to extract teeth. When pocketing or gingival recession exceeds 50% of the root support, extraction is indicated and should be performed by trained veterinarians or referred for treatment by a veterinary dental specialist when the practitioner does not have the expertise, equipment, or facilities to perform treatment. It is recommended that extraction sites >1 mm should be sutured with absorbable suture (4-0 or smaller) to keep blood clots in and food and debris out.
8. +/- Antibiotic therapy
Administer either systemic or local perioperative antibiotics where indicated. The use of antibiotics in veterinary dentistry must be assessed on a case-by-case basis. Therapeutic antimicrobials should be used appropriately in the surgical setting. Most dental procedures are considered to be clean-contaminated procedures, meaning that after extractions, systemic antibiotics are usually not indicated.45–47
Preoperative antibiotics given several days before surgery may be administered in cases of PD4 for the purpose of making tissues more amenable to surgical handling. Intraoperative antibiotics may be indicated in patients with systemic risk factors, such as subaortic stenosis, systemic immunosuppression, and orthopedic implants placed in the last 12–18 mo. Appropriate clinical judgment for each individualized patient is necessary. Postoperative antibiotics are indicated when radiographic evidence of presumed osteomyelitis is present. Clindamycin (5.5 mg/kg per os q 12 hr) and amoxicillin-clavulanic acid (13.75 mg/kg per os q 12 hr) are both approved for use in cases of dental infections and should be prescribed for a full 7–14 day course.
The use of locally applied antimicrobials (LAA), also called perioceutics, may be indicated where a >5 mm cleaned pocket exists in PD2 or PD3 cases (Figure 9). The purpose of use is to improve periodontal health and encourage reattachment to a normal level.48 PD4 cases require more invasive periodontal debridement and management; however, locally applied antimicrobials (LAA) may also be a component.

FIGURE 9 Injection of perioceutic into a 5 mm cleaned, bleeding periodontal pocket. Photo courtesy of Jan Bellows.
9. Antiplaque sealant application
Apply antiplaque substances such as barrier sealants. It is important for practitioners to understand the appropriate indications for the use of sealants. The term “sealant” in human dentistry is a substance applied to teeth to prevent tooth decay. In veterinary medicine, barrier sealants are applied to decrease the accumulation of plaque (Figure 10).
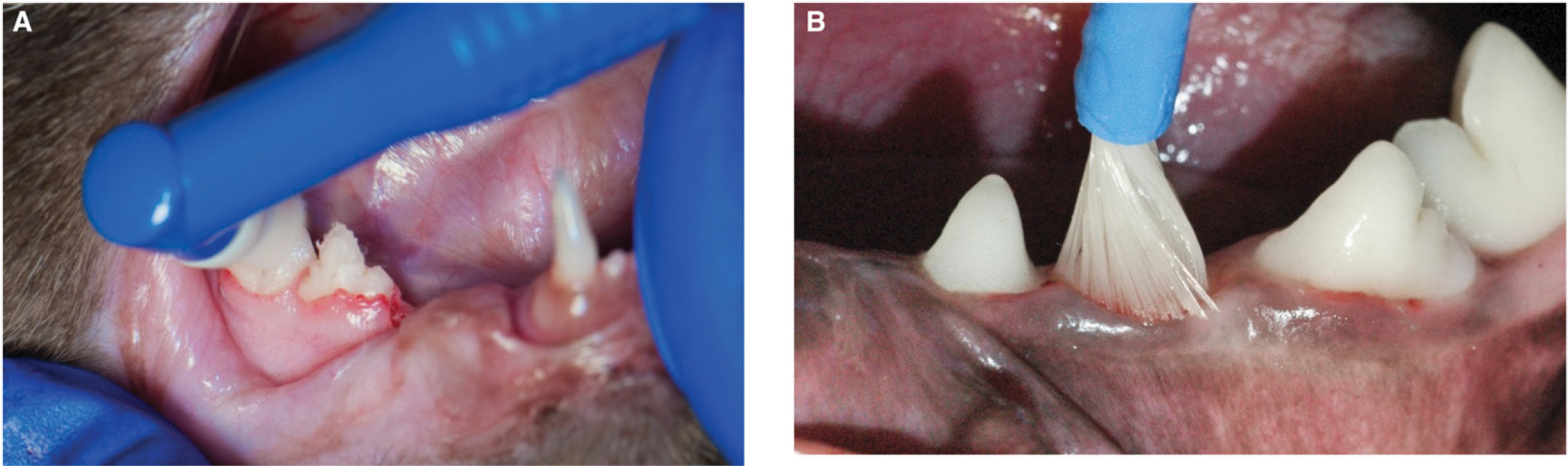
FIGURE 10 - Application of antiplaque sealant.
(A) Barrier sealant gel professionally applied to a cat’s gingival sulcus; home plaque prevention gel is then reapplied weekly by the pet owner.
(B) Application of hydrophilic gingival dental sealant professionally applied to a dog’s gingival sulcus; reapplication is recommended every 6 mo.
Photo courtesy of Jan Bellows.
Although the use of barrier sealants has been shown to decrease accumulation of plaque subgingivally, it does not totally prevent accumulation of subgingival plaque, the occurrence of periodontal disease, the need for home oral hygiene, or professional dental therapy.49–51
The use of resin-bonded sealants is designed to treat damaged tooth structure (e.g., fractured or abraded teeth without pulp exposure) by sealing exposed dentin tubules, thus decreasing sensitivity and risk for bacterial migration leading to pulpitis. A complete examination and intraoral radiographs are necessary before using any bonded sealant to identify nonvital teeth and other pathology. Application of these products requires appropriate training and radiographic follow-up in 6 mo to reconfirm tooth vitality. Inappropriate use may result in increased dental pain, risk for infection, and loss of tooth vitality. The use of resin-bonded sealants in cases of tooth resorption is contraindicated.52,53
10. Oral mass biopsies
Biopsy all abnormal masses visualized grossly or radiographically and submit samples for histopathologic evaluation by a pathologist qualified in oral tissues analysis.54
11. Anesthesia recovery
Maintain an open airway via intubation until the animal is swallowing and is in sternal recumbency. Maintain body temperature and continue intravenous fluid support as needed. Continuously monitor and record vital signs until the patient is awake. Continue pain management while the pet is in the hospital and upon discharge.55–57
12. Home care education
Provide instruction on home oral hygiene. See the section on Oral healthcare. The Veterinary Oral Health Council (VOHC) lists products that have been scientifically proven to be effective in retarding accumulation of dental plaque and/or calculus.58,59



