Patient considerations
Identifying the hospice and palliative care patient
The overarching goal in providing palliative and hospice care is to maximize comfort and minimize suffering for our patients.
Canine and feline patients who are candidates for hospice or palliative care generally have at least one or a combination of the following conditions: a terminal diagnosis; a chronic progressive disease (e.g., end-stage renal disease, debilitating osteoarthritis, congestive heart failure); a progressive, undiagnosed disease; a chronic disability (e.g., neurologic or intervertebral disk disease); or terminal geriatric status, exemplified by wasting or failure to thrive.6,7 When developing a hospice or palliative care treatment plan to be executed by an interdisciplinary team, it can be helpful to assign the patient to one of the following categories:
- Diagnosis of life-limiting disease
- Decision not to pursue diagnosis or curative treatment
- Curative treatment has failed
- Clinical signs of chronic illness that interfere with normal routine or QOL
- Progressive illness with complications
These broad case descriptions are useful for managing the client’s expectations as well as developing a treatment plan.
Medical conditions appropriate for hospice or palliative care
- Terminal diagnosis
- Chronic, progressive disease
- Progressive, undiagnosed disease
- Chronic disability
- Terminal geriatric status
The animal hospice care pyramid
A patient’s passage from palliative to hospice care and, ultimately, to death is a progression that can range from hours to months to complete. As with human medicine, the physical, social, and emotional health of veterinary patients is strongly interrelated. It is difficult to achieve optimal QOL when any one of these components is missing. The Animal Hospice Care Pyramid (Figure 1) illustrates these complementary areas of patient care that should be considered during the EOL transition. Each level of the pyramid builds upon the others to achieve optimal EOL experiences. The base of the pyramid includes the animal’s physical wellbeing that represents the traditional clinical care services that veterinarians provide. However, successful management of the hospice patient must also consider the mid-level of the pyramid consisting of the social welfare of the pet, and the pyramid apex that focuses on the pet’s emotional wellbeing. When the healthcare team, working in collaboration with the pet owner, successfully addresses all three levels of the hospice care pyramid—physical, social, and emotional needs—the practice is best able to maximize comfort and minimize suffering. Those are, after all, the ultimate goals for every pet that has entered into its EOL stage. Table 1 lists important issues that need to be addressed at each level of the Animal Hospice Care Pyramid.
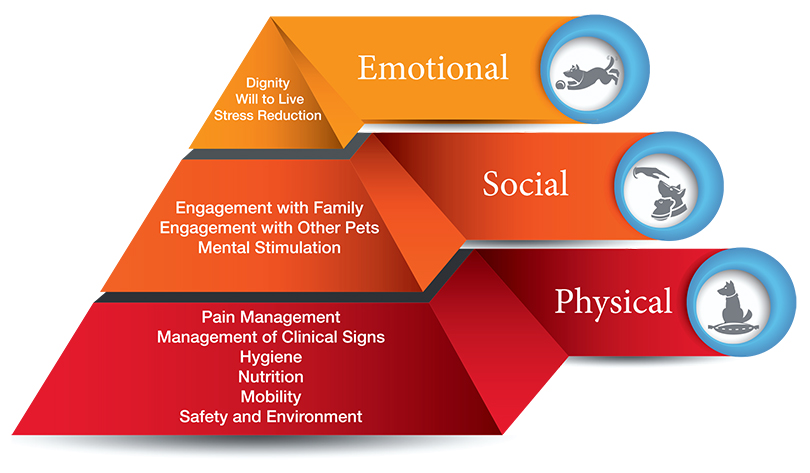
FIGURE 1 Animal Hospice Care Pyramid. Veterinary hospice care can be segmented into a hierarchy of three components, each of which must be satisfactorily addressed to provide optimum end-of-life (EOL) care. The base of the pyramid consists of physical care, the traditional acute and chronic care services provided by veterinarians. The midlevel consists of the patient’s social wellbeing, centering on interaction with other pets and humans. The apex of the pyramid consists of the patient’s emotional wellbeing, including satisfaction of the individual animal’s unique set of needs and a meaningful engagement with her or his surroundings.8 Illustration Design: Shea Cox, DVM
TABLE 1: Components of an integrated approach to end-of-life (EOL) care
Physical care
| Objective | Intervention |
|---|---|
|
Pain management |
Anticipate, prevent, control, and regularly monitor acute and chronic pain; provide multimodal pain relief per 2015 AAHA/AAFP Pain Management Guidelines for Dogs and Cats:28
|
|
Management of clinical signs |
Examine patient to diagnose and treat dyspnea, GI signs, cognitive dysfunction, anxiety, pruritus and skin integrity (e.g., local infections, pressure sores), dental health, respiratory signs |
|
Hygiene |
Maintain urine and feces sanitation, access to elimination sites |
|
Nutrition |
Perform dietary and body condition assessment; monitor dietary habits and changes; maintain balanced nutrition, adequate food intake, and hydration to the extent possible, keeping in mind that decreased food and water intake are normal in the dying process |
|
Mobility |
Provide nonskid flooring in pet’s living area, accessible litter box location and design, physical assistance devices (harnesses, slings, carts, and wheelchairs), range-of-motion exercises |
|
Safety |
Restrict access to environmental hazards (e.g., swimming pools), protect from aggressive pets, observe for self-trauma |
|
Environmental needs |
Provide comfortable bedding, temperature and ventilation control, adequate space, peaceful environment |
Social wellbeing
| Objective | Intervention |
|---|---|
|
Engagement with family |
Involve pet in family activities as illness allows, maintain regular owner-pet interaction |
|
Isolation avoidance |
Avoid or minimize extended periods of isolation or non-socialization |
|
Interaction with other pets |
Maintain appropriate interaction with other pets, monitor pet-to-pet hierarchal changes and adverse socialization behaviors |
|
Mental stimulation |
Offer regular play opportunities and environmental enrichment |
Emotional wellbeing
| Objective | Intervention |
|---|---|
|
Preservation of dignity |
Minimize house soiling, manage incontinence, maintain good hygiene and grooming |
|
Stress reduction |
Minimize exposure to stress and changes in routine, assess pet’s willingness to receive needed treatments |
|
Preserve pet’s household role |
Continue expectations for companionship, surveillance, or other household roles; adhere to daily routines |
|
Maintain the will to live |
Monitor behavior; ensure regular interaction with family members; observe for signs of withdrawal, depression, or resignation |
TABLE 2: Practical issues in implementing a palliative or EOL care plan
Issues and topics to discuss with client
| Issue | Topics to Discuss with Client |
|---|---|
|
Treatment locations |
|
|
Individual responsibilities |
|
|
Client education |
|
|
Environmental modifications |
|
|
Owner safety and hygiene |
|
|
Periodic plan assessments |
|
|
Medication, nutrition, and activity review and assessment |
|
Developing a treatment plan for palliative and hospice care
By using the following four-step process, the practice team will be able to implement a consistently effective palliative and hospice care treatment plan for EOL patients:
Step 1: Educate the Client about the Pet’s Disease
Educating clients about the patient’s disease is particularly important in EOL cases.9 The more the caregiver understands about the disease progression, the better he or she will be able to cope with their expanded, EOL caregiving role. The veterinarian should advise the client about the expected trajectory of the pet’s disease. This should include a discussion of diagnostic and treatment options, interventions to ensure the pet’s comfort, and a realistic prognosis. One of the goals of client education in EOL cases is for the client to have a clear understanding of all diagnostic and treatment options. Decisions on EOL care should be made only when the client has achieved a clear understanding of the options.
Clients should be advised that some diagnostic procedures, such as biopsies, might be painful for the pet. A thorough description of each diagnostic test, including how the results will influence patient care, will allow the client to make an informed choice about whether or not to authorize the procedure. The veterinarian should describe the diagnostic tests and therapies in a language that the client can understand and minimize the use of clinical terminology, abbreviations, or acronyms that can be overwhelming or intimidating to client. Effective client education about EOL care includes the cost of services and avoids giving false hope.
The best time to discuss the pet’s disease with the client is not necessarily when the individual is informed of a terminal or progressive disease diagnosis for the patient. Depending on the degree of attachment between the pet and its owner, the impact of such news will often evoke a strong emotional reaction in the owner. Practitioners should anticipate this reaction, respond to it by expressing empathy, and consider setting up a follow-up appointment to discuss EOL treatment options. This gives the owner time to come to terms with the new reality and to participate more fully in the development of a realistic, mutually acceptable treatment plan. The follow-up visit is an opportunity for a two-way information exchange between the veterinarian and client. An effective approach for conducting an EOL follow-up discussion is to schedule the appointment at the end of the day or as the last appointment before the lunch hour, giving the veterinarian and client time for an uninterrupted, open-ended discussion.
Take-Away Points
- It is important to advise clients about the expected disease trajectory.
- Ensure that there is a clear understanding of all diagnostic and treatment options available.
- Consider scheduling a dedicated EOL appointment 1 wk after the need for hospice care has been identified.
Step 2: Evaluate the Pet Owner’s Needs, Beliefs, and Goals for the Pet
Whether conducted at a follow-up visit or at the time a terminal diagnosis is communicated to the client, it is important for the practitioner to explore the client’s needs, beliefs, and goals for the patient’s EOL care.10 Treatment goals described by the client should be as specific as possible and recorded in detail in the patient’s medical record. It is often helpful to have a checklist of questions to ask and issues to discuss with the client as the basis for developing a personalized EOL treatment plan for their pet. Table 2 provides a list of issues to discuss with the client when an EOL or palliative care treatment plan is developed. This inventory of practical concerns can be used as a resource during periodic exams or consultations with the client. The list will help the practitioner and client to assess the patient’s status, evaluate treatment plan efficacy, and revise the plan based on the patient’s response and the client’s willingness and capacity for implementing the plan. The discussion should focus on how to achieve a balance between QOL and duration of life, goals for pain management, and whether euthanasia or natural death is the preferred option.
Understanding the client’s viewpoints towards EOL care for the patient places a premium on effective listening skills. In addition, maintaining eye contact, displaying empathetic body language, and repeating in your own words what the client is saying are core communication techniques.11 The client should be invited to ask questions and should not feel rushed or pressured into making treatment decisions. Regardless of the decisions that are made, the client should never feel judged.
Step 3: Develop a Personalized EOL Treatment Plan
Developing an effective, patient-specific EOL care treatment plan is a collaborative effort involving the veterinary staff and the client. In general terms, there are two paths available for EOL care: (1) aggressive care, which seeks to extend the duration of life; and (2) palliative care, which seeks to maintain the patient’s best possible QOL. These approaches are not mutually exclusive. An aggressivecare treatment plan can, and should, place significant emphasis on QOL. The veterinarian has an obligation to consider the appropriateness of specific care recommendations. This includes answering the hard question: “Just because we can do something medically, does that mean we should?” This is a question that should be discussed during collaborative decisionmaking with the client.12 For terminal cases, not all aggressive interventions are in a patient’s or owner’s best interest. For example, performing radical surgery requiring a significant amount of rehabilitation may not be in the patient’s best interest if expected survival time is short. The goal of collaborative decisionmaking is to identify options that are reasonable from the standpoint of both the patient and the owner. In addition, it is important for the veterinarian to assess the current nutritional status of the patient (body condition score, muscle mass index) and develop a workable nutritional plan for the patient in consultation with their owner. It should be expected and explained that inappetance and anorexia are real concerns in hospice care and that specialized diets are available for use in critical or cachectic patients. Early intervention, whether through assisted feeding or appetite stimulants, may need to be offered, but with consideration to the fact that reduced food and water intake is normal in the dying process.
Consulting with a veterinary nutritionist could also be of benefit to assess the patient’s specific nutritional needs and to assist in the feeding plan.
All EOL treatment plans start with a thorough assessment of the patient and his or her medical, social, and emotional needs. These may include, but are not limited to:
- Organ system disease or failure and associated signs, including the special senses
- Pain (location, cause, severity, and ability to control)
- Difficulty eating and drinking
- Decreased oxygenation or difficulty breathing
- Elimination problems
- Mobility limitations
- Tumor disease or tumor activity
- Current mood (relaxed versus anxious, happy versus depressed)
- Need for and availability of companionship (humans and other animals)
- Engagement with her or his surroundings
- Emotional and cognitive status
When developing an EOL care treatment plan, the practitioner should discuss with the client his or her ability and willingness to provide the increased level of caregiving generally required for a terminal patient. The client’s capacity for caring for their pet is an important consideration in developing the treatment plan since it relies on the owner’s active involvement. Allowing time to hear the client’s questions and concerns and the extent to which the client can provide supportive care is essential in collaboratively selecting the best course of treatment.
A proposed palliative care plan should be detailed, but it should be presented in language that the client can understand without over-reliance on medical terminology. The plan and the logistical implications for the owner should be discussed and agreed upon. Because of the sensitive nature of EOL care, it is critical for the client to make an informed decision regarding their pet’s treatment plan. The treatment plan should be entered into the patient’s medical record. Treatment plan components should include:
- Patient care procedures assigned to the owner based on the individual’s capability and willingness to assume specific responsibilities for care.
- An assessment of the patient’s willingness and capacity to receive care. This would also include the patient’s willingness to eat, or the indication for the need for supplemental nutrition (i.e., feeding tubes or syringe feeding) or stimulation of appetite (e.g., mirtazapine).
- A written action plan, which has been discussed point-bypoint, with the owner, to ensure their active participation.
- An estimate of the time required for the owner to execute those parts of the plan for which they are responsible.
- An estimate of costs itemized by fees for professional services and costs of medication, supplies, and nutritional products.
- A schedule for follow-up communication and reassessment.
Take-Away Points
- Collaboratively with the caregiver, hospice options that are reasonable for both the caregiver and the patient need to be determined.
- It is important to provide a detailed EOL care plan using language that caregivers can understand.
Step 4: Implement Palliative or Hospice Care
Whenever possible, palliative treatment and EOL care should be administered at home. This generally involves instructing the client on therapeutic techniques, how to assess the patient’s response, and clinical sign recognition. The home environment should be evaluated to ensure the patient’s comfort and safety during EOL treatment. Environmental modification or enrichment might include modifying floor surfaces, improving accessibility to food and water, ensuring that bedding is comfortable, optimizing litter box location and design, selecting an ideal ambient temperature, and maintaining sanitation and hygiene. The client should be instructed in the safe handling of their pet to prevent injury to self and the pet, as well as safe handling of owner-administered medications. Technologies such as video recording or video conferencing can be helpful in regularly communicating the patient’s home-care status with the veterinary healthcare team.
Bioethical considerations
End-of-life case management and dialogue with the client about the patient’s treatment options should be guided by the four principles of medical bioethics: (1) respect for autonomy, (2) nonmaleficence, (3) beneficence, and (4) justice. These principles are described in a definitive and recently updated textbook by Beauchamp and Childress, Principles of Biomedical Ethics.13 As an EOL case progresses and the client’s attitudes toward their pet’s response to treatment evolve, the veterinarian may need to reconsider the balance between the four bioethical principles and adjust the treatment plan accordingly. One bioethical principle may take precedence over another. For example, when an animal is uncooperative for administration of analgesics (autonomy versus beneficence) or when analgesics administered cause adverse reactions (beneficence versus non-maleficence). It is important to acknowledge that this may occur and to be prepared to justify infringing on one bioethical principle in order to adhere to another. All four principles can apply to both the caregiver and the patient.
Respect for autonomy, as it applies to clients, is the obligation of the veterinary medical professional to disclose the information needed for a client to make the best decision on behalf of their pet. Although the client’s medical knowledge may be limited, they can still make informed decisions and exercise control over their pet’s treatment plan when the veterinary team explains outcomes clearly and completely. Actions by the team that support respect for the autonomy of the client include being truthful; respecting the client’s values, beliefs, culture, privacy, and confidentiality; obtaining consent before performing any treatments; and helping to direct decisionmaking when asked.
Respect for autonomy also implies consideration of the patient’s autonomy. Animals can become fearful and lonely, anticipate pain, and express preferences. These affective (emotional) states are important in palliative and EOL care. In order for EOL care to be successful, not only must the client be willing and able to implement the treatment plan, the patient must also be a willing participant. This is analogous to delivery of medical care to children. The parent is the decisionmaker when pediatric care is involved, just as the owner is the decisionmaker in companion animal medicine. Similar to children now routinely being included in their medical care at a level appropriate to their development, pets can and should be included in their EOL care by respecting the preferences they express about receiving care. Examples include cats jumping onto the counter versus disappearing under the bed when it is time for medication administration; non-ambulatory dogs expressing their pleasure when taken out for a wagon ride; and cats who will bite, scratch, or climb walls rather than go into their carrier.
Non-maleficence is the bioethical principle of “do no harm.” Non-maleficence in palliative and EOL care translates into avoiding iatrogenic escalation of discomfort and pain experienced by patients because of clinical intervention. Examples are skin reactions at the site of transdermal patch application, persistent postoperative pain, or depression induced by hospitalization. Non-maleficence also includes avoiding negligence in the form of deviating from the accepted standard of care. Non-maleficence towards the caregiver includes avoiding insensitive conduct and inadequate communication by veterinary staff that can aggravate the caregiver’s grieving experience. Non-maleficence is complemented by the bioethical principle of beneficence, or deliberate interventions that benefit the patient and/or their caregiver.
Beneficence toward the caregiver may consist of open and honest discussions about the patient’s prognosis and cost of care during the EOL stage. Beneficence toward the patient may involve discussing euthanasia in cases when continuing treatment will result in suffering.
The last of the four bioethical principles is justice, which implies fairness. It is just for the practitioner to provide all clients with their best effort on behalf of the pets, regardless of the client’s background. It is equally just to treat individual patients based on their preferences as well as the client’s financial resources, commitment to the treatment plan, and compliance with recommendations.
Take-away points
- Treatment options should be guided by the four principles of medical bioethics.
- The veterinary team may need to adjust the treatmentplan accordingly as an EOL case progresses.
- Treatment options and clinical interventions should alwaysreflect the bioethical principle of “do no harm.”



